There are a number of symptoms you should look out for, including:
- headache
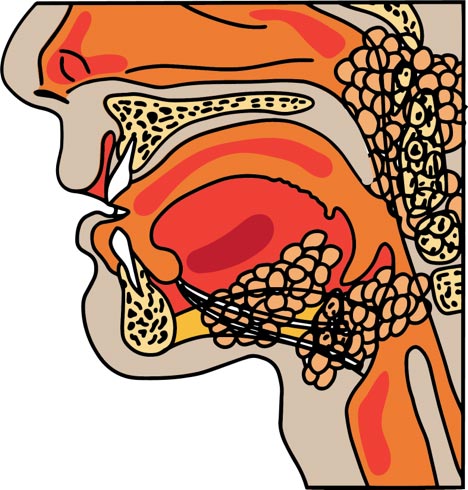
- pain in your mouth, upper teeth, throat, neck, face, or chin
- a lump, sore and/or a mouth ulcer that does not go away
- unusual bleeding in your mouth, blood in your spit, or coughing up blood
- a sore throat with earache especially just on one side
- any changes to your voice especially a hoarse voice, or a constant cough
- white or red patch inside your mouth, lumps in the neck or near glands that are there for longer than 2 weeks
- trouble or pain talking, swallowing, seeing, smelling things normally or breathing
- losing weight without trying.
Having these symptoms may not mean you have cancer, but it is really important to check.
If you have any of these problems, or are worried about something else, yarn with your doctor, nurse or Aboriginal and/or Torres Strait Islander health worker.