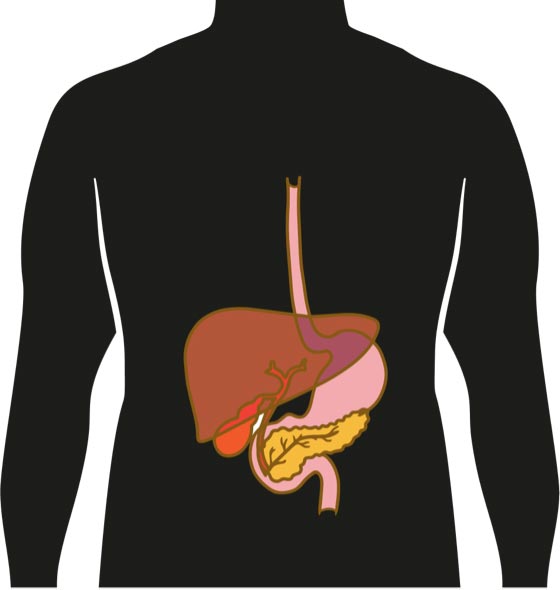
There are a number of symptoms you should look out for, including:
- skin colour, and/or the whites of your eyes changing to yellow (jaundice)
- ache or pain on the right side of your belly
- a swollen belly (ascites)
- hard lump on your right side, below where your ribs stop
- pain in your upper back, around the right shoulder blade
- losing weight without meaning to
- pale stools or dark coloured pee
- feeling really tired
- loss of appetite and/or nausea
Having these symptoms may not mean you have cancer, but it’s important to check.
If you have any of these problems, or are worried about something else, yarn with your doctor, nurse or Aboriginal and/or Torres Strait Islander health worker.